Changing health care
to improve quality of
life for all.
Beth Israel Lahey Health’s roots in providing top-quality health care date back nearly a century. We're fully committed to ensuring our patients receive the care they deserve. As a leading healthcare provider throughout New England, we aim to change the current state of health care for the better and make lasting improvements that guarantee access to our services.
Coding and Billing Analyst
Burlington, Massachusetts
Organization Facility: Beth Israel Lahey Health - Non Executive Category: Billing, Collections, & Patient Financial Services Job ID: JR81454 Date posted: 08/12/2025Job Type: Regular
Time Type: Full time
Work Shift: Day (United States of America)
FLSA Status: Exempt
When you join the growing BILH team, you're not just taking a job, you’re making a difference in people’s lives.
Reporting to the Coding and Billing Manager, the Coding and Billing Analyst serves as the preeminent analytical coding resource tasked with improving revenue results and operational efficiencies throughout the professional billing revenue cycle for all One BILH professional billing entities. Due to its wide scope of clinical specialties, complex front to back-end billing functions and workflows, this position requires an advanced-level knowledge of the utilization of ICD-10 and CPT coding principles in the assignment and sequencing of diagnostic and procedure billing codes, including current knowledge of third party payer documentation requirements. The Coding and Billing Analyst analyzes and performs functions related to professional coding and activities as they relate to system-wide quality, improvements, revenue cycle/systems workflows and above all quality coding functions. Responsible for oversight of Quality Assurance by conducting regular staff audits to ensure that complex specialized and unique workflows are coded with accuracy. Due to its service focus and project management emphasis, this position requires strong interpersonal and communication skills, well-developed analytic and organizational skills. Provides quality customer service and serves as an exemplary representative of the Patient Financial Services team.Job Description:
Essential Duties & Responsibilities including but not limited to:
1. Proven analytical skills needed to analyze coding for each complex specialty. Locate patterns and trends by focusing on high volume denials that have a common denominator. Analyze root cause and determine where efforts need to focus; physician documentation, charging, system edits, payer billing guidelines, workflows etc. Recommending and implementing a course of action to resolve denial.
2. Assists in developing mechanisms for internal staff auditing. Under managerial oversight develops necessary resources to ensure optimal performance and service delivery excellence. Supports the maintenance a system of reporting that provides timely and relevant information on all aspects of audits and compliance issues to management.
3. Assists the manager in monitoring coding related accounts receivable across all BILH entities, effectively through weekly/monthly reporting mechanisms to ensure key performance indicators are within established goals and national benchmarks. Identifies trends and conducts root cause analysis. Makes recommendations to close identified gaps in processes, people, or technology.
4. Works with staff to ensure compliance of, and proper coding technique as defined by CMS regulations, Local Medicare Review Policies (LMRP’s), Local Carrier Determinations (LCD’s), the AMA, any applicable BILH compliance policies, and/or any relevant accrediting organizations. Provides ongoing coding education as well as new coder education on proper coding and documentation.
5. Acts as a Liaison between PFS and the Professional Coding Department by communicating issues, payer policy changes related to coding and opportunities to increase revenue and reduce denials as appropriate.
6. Facilitates the escalation of payer issues and reporting for every BILH entity and follow through of issue resolution of BILH assigned payer provider representatives.
7. Establishes and maintains effective working relationships with each BILH entity’s clinical departments and administrative leadership.
8. Works with the department manager to coordinate the management of quality levels, timeliness in the performance of transactions, the resolution of edits and control of backlogs for each BILH entity.
9. Attends appropriate organizational and industry meetings to develop and maintain necessary Professional and Technical Coding knowledge as well as stays current will all billing regulations as they relate to coding. Follows all CMS, AMA, AHA, CPT, ICD-10, HCPCS, coding and billing guidelines.
10. Assists the manager is developing new workflows and department strategies for new technology, changing payer and regulatory environments for each BILH entity.
11. Collaborates with Directors, Managers, and Leads to create a working environment that ensures success at all levels across PFS and actively participates and contributes to PB revenue cycle operational workflow decisions. Contributes to new training curriculum and course material updates for responsible areas.
Minimum Qualifications:
Education: Associate Degree or Equivalent Health Experience Required
Licensure, Certification & Registration: Coding Certificate from College Level Coding Program, and CPC, CCS-P, COC, or CCS required.
Experience: 3+ years in healthcare environment preferably in a professional billing environment.
Skills, Knowledge & Abilities: The knowledge and abilities required to perform this function would typically be acquired through training and experience equivalent to graduation from an accredited school with an Associate degree; comprehensive knowledge of the components associated with billing for a large multi-specialty academic group practice. Excellent verbal and communication skills along with the ability to maintain productive and professional relationships. Excellent problem identification and solving skills. Works independently, ability to prioritize and organizational skills a must. Excellent communication skills.
As a health care organization, we have a responsibility to do everything in our power to care for and protect our patients, our colleagues and our communities. Beth Israel Lahey Health requires that all staff be vaccinated against influenza (flu) as a condition of employment. Learn more about this requirement.
More than 35,000 people working together. Nurses, doctors, technicians, therapists, researchers, teachers and more, making a difference in patients' lives. Your skill and compassion can make us even stronger.
Equal Opportunity Employer/Veterans/Disabled
Featured Jobs
-

-

-

-

-
 Check out Benefits at BILH
Check out Benefits at BILHDiscover the outstanding BILH benefits that await you, encompassing competitive compensation packages, healthcare coverage, and a range of wellness programs designed to support your overall well-being.
-

-

-

-

-

-
 Saved Jobs
Saved JobsView and manage your saved jobs
-

-
 Learn more about Nursing at BILH
Learn more about Nursing at BILHExplore the diverse and rewarding nursing opportunities at BILH, where you can make a meaningful impact on patient care while growing your skills in a supportive and innovative healthcare environment.
-

-
 New Grad and Newly Licensed Nursing Program
New Grad and Newly Licensed Nursing ProgramAs new grad or newly licensed RN, explore the rotational programs at our hospitals.
-
 Learn more about Nursing at BILH
Learn more about Nursing at BILHExplore the diverse and rewarding nursing opportunities at BILH, where you can make a meaningful impact on patient care while growing your skills in a supportive and innovative healthcare environment.
-
 Explore Upcoming Events
Explore Upcoming EventsStay informed and engaged by exploring the upcoming BILH events, where you'll have the opportunity to connect with colleagues, expand your professional network, and gain insights into the latest advancements and trends in healthcare.
-
 Learn more about Operating Room roles at BILH
Learn more about Operating Room roles at BILHExplore the many Operating Room nurse and surgical tech opportunities at BILH, where you can make a meaningful impact on patient care while growing your skills in a supportive and innovative healthcare environment.
-
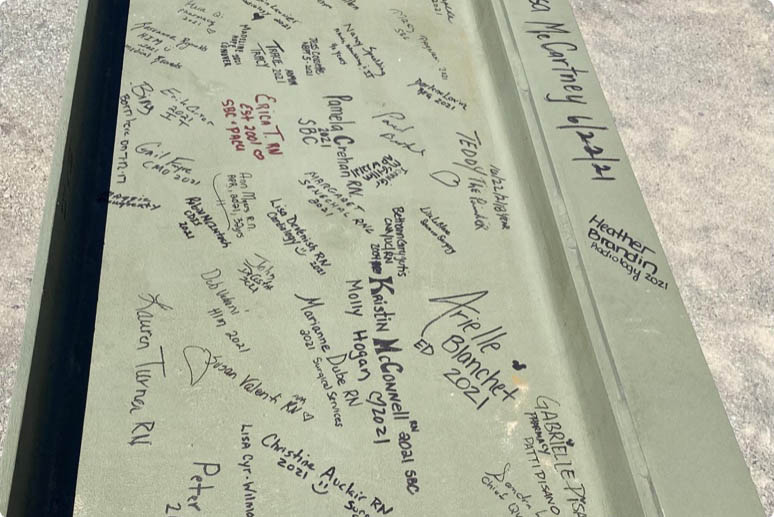
 Explore open positions within our Radiology Team at BILH!
Explore open positions within our Radiology Team at BILH!Beth Israel Lahey Health has multiple opportunities to join the Radiology team. Join a work place that strives for excellence!
-

-
 Our Allied Health Team
Our Allied Health TeamLearn more about Allied Health job opportunities
-
 Job Opportunities: Woburn, MA
Job Opportunities: Woburn, MALearn more about job opportunities at BILH in the Woburn, Massachusetts area
-

Why join Beth Israel Lahey Health?
If you’re looking for a career where you can make a difference and explore your potential, Beth Israel Lahey Health is the place you belong. Our system includes a network of hospitals, physician practices, outpatient centers, and other healthcare facilities and we offer a broad range of careers in direct patient care, environmental services, registration, finance and many other fields. We are focused on providing compassionate and personalized healthcare with a strong reputation for clinical excellence and research and offer diverse opportunities for career growth and development. Conveniently, we have many locations in communities across Eastern Massachusetts and Southern New Hampshire.
At Beth Israel Lahey Health, we see you for all that you are – your experience and your dreams. Explore our open opportunities and find out why so many have already chosen to join our team.
View All Opportunities