Changing health care
to improve quality of
life for all.
Beth Israel Lahey Health’s roots in providing top-quality health care date back nearly a century. We're fully committed to ensuring our patients receive the care they deserve. As a leading healthcare provider throughout New England, we aim to change the current state of health care for the better and make lasting improvements that guarantee access to our services.
Credentialing & Insurance Specialist
Charlestown, Massachusetts
Organization Facility: Beth Israel Lahey Health - Non Executive Category: Credentialing / Medical Staff Services Job ID: JR81396 Date posted: 07/28/2025Job Type: Regular
Time Type: Full time
Work Shift: Day (United States of America)
FLSA Status: Non-Exempt
When you join the growing BILH team, you're not just taking a job, you’re making a difference in people’s lives.
The CVO Insurance and Credentialing Specialist shall be responsible for managing end to end aspects of the CRICO malpractice insurance program for BILH employed and sponsored providers—ensuring accurate eligibility, classification, activation, and termination of coverage in accordance with organizational policy and regulatory standards.In addition, the CVO Insurance and Credentialing Specialist shall assist in the credentialing and re-credentialing process for providers across the BILH system, as assigned. This includes coordination of sending, receiving, processing, and primary source verification of applications for initial appointment, reappointment, and their associated clinical privilege.
The CVO Insurance and Credentialing Specialist exemplifies a culture of excellence, professionalism, effective communication, and customer service. They collaborate closely with CVO leadership and staff, internal and external stakeholders, providers, and clinical and administrative leaders to ensure timely, accurate, and compliant credentialing and professional malpractice insurance enrollment.
This individual must handle significant, complex, multidisciplinary, and confidential matters with discretion and sound judgment. A strong understanding—or the ability to develop a strong understanding—of insurance, provider credentialing, and medical staff operations and the unique cultures of each affiliated institution is essential. The CVO Insurance and Credentialing Specialist actively works to find common ground and support the development of a unified, system-wide culture of excellence and operational efficiency.
Job Description:
Essential Duties & Responsibilities including but not limited to:
In accordance with established CVO policies and procedures for assigned hospitals, the CVO Insurance and Credentialing Specialist shall include the following:
- Manages the CRICO malpractice insurance process for BILH employed and sponsored providers across the system, ensuring timely and accurate onboarding, eligibility verification, coverage activation, and termination.
- Serves as the primary liaison between the CVO, CRICO, and system stakeholders to coordinate provider coverage and resolve any discrepancies.
- Maintains up-to-date documentation and reporting related to malpractice insurance status in accordance with organizational and regulatory requirements.
- Works collaboratively with Human Resources, Legal, and Medical Staff Offices to ensure seamless integration of insurance management within the credentialing lifecycle.
- Monitors policy renewals, expirables for all active insurances (regardless of carrier and type), identifies gaps in coverage, and initiates corrective actions as needed to ensure continuous and compliant insurance coverage for all applicable providers.
- analyzing verification information, to include identifying red flag and/or adverse information and notifying CVO leadership in accordance with CVO policies
- monitoring of expiring information such as, but not limited to, federal and state DEA, state professional license(s), professional liability insurance, and specialty board certification status
- maintain and update credentials file(s) (paper and/or electronic as applicable)
- timely, accurate, and complete database entries
- maintenance of electronic files as required
- appropriately and timely communicate with supervisor regarding status of credential applications
- timely and accurately prepare credential files for audit and submission to assigned hospitals
- participate in peer to peer credential file audits, as needed and assigned
- compliance with standard turn-a-round times
- maintain a general working knowledge of relevant regulatory standards (i.e., TJC and NCQA), state and federal requirements.
- participation in special project teams as assigned
- continually strives to achieve individual, team and departmental goals
Organizational Requirements:
1. Maintain strict adherence to the BILH CVO Confidentiality policy.
2. Incorporate BILH CVO Standards of Behavior and Guiding Principles into daily activities.
3. Comply with all BILH CVO Policies.
4. Comply with behavioral expectations of the BILH CVO.
5. Maintain courteous and effective interactions with colleagues, providers, and BILH leadership.
6. Demonstrate an understanding of the job description, performance expectations, and competency assessment.
7. Demonstrate a commitment toward meeting and exceeding the needs of our customers and consistently adheres to BILH CVO customer service standards.
8. Participate in departmental and/or interdepartmental quality improvement activities.
9. Participate in and successfully completes Mandatory Education.
10. Perform all other duties as needed or directed to meet the needs of the department.
Minimum Qualifications:
Education:
- High School Diploma or higher
Licensure, Certification & Registration - Preferred:
- NAMSS CPCP or CPMSM Certified
- or
- Certified Administrative Professional
Experience:
- Minimum of 3 years of experience in a healthcare setting required.
Prior experience in one or more of the following roles is strongly preferred:
- Credentialing Specialist in a Credentialing Verification Office (CVO) or Medical Staff Office, with demonstrated knowledge of credentialing standards, provider data management, and regulatory requirements (e.g., Joint Commission, NCQA)
- Executive Administrative Assistant supporting hospital or healthcare system leadership, with experience managing sensitive information, coordinating meetings, and maintaining organized documentation.
- Finance or Risk Management professional responsible for overseeing or supporting the administration of provider malpractice insurance, including policy tracking, eligibility monitoring, and coordination with external carriers (e.g., CRICO, commercial insurers)
Skills, Knowledge & Abilities:
- Knowledge of credentialing software and associated applications strongly preferred.
- Excellent interpersonal and communication skills
- Ability to work under minimal supervision and to adapt quickly to changes within the environment
As a health care organization, we have a responsibility to do everything in our power to care for and protect our patients, our colleagues and our communities. Beth Israel Lahey Health requires that all staff be vaccinated against influenza (flu) and COVID-19 as a condition of employment. Learn more about this requirement.
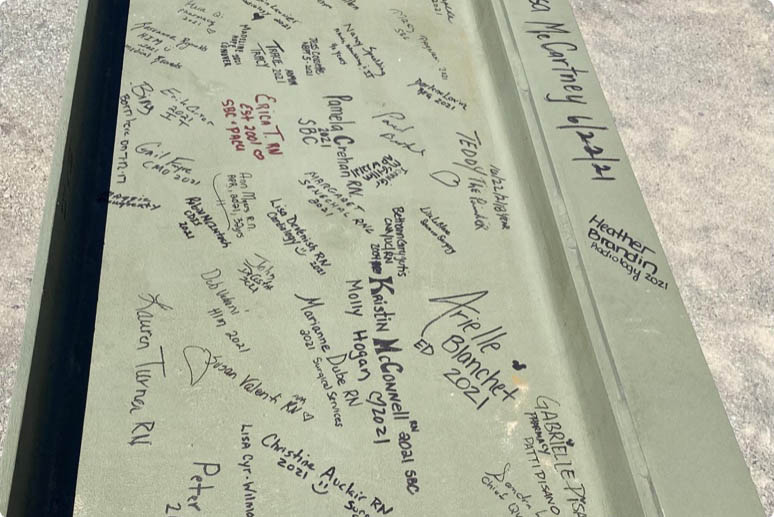
More than 35,000 people working together. Nurses, doctors, technicians, therapists, researchers, teachers and more, making a difference in patients' lives. Your skill and compassion can make us even stronger.
Equal Opportunity Employer/Veterans/Disabled
Featured Jobs
-

-

-

-

-
 Check out Benefits at BILH
Check out Benefits at BILHDiscover the outstanding BILH benefits that await you, encompassing competitive compensation packages, healthcare coverage, and a range of wellness programs designed to support your overall well-being.
-

-

-

-

-

-

-

-
 Learn more about Nursing at BILH
Learn more about Nursing at BILHExplore the diverse and rewarding nursing opportunities at BILH, where you can make a meaningful impact on patient care while growing your skills in a supportive and innovative healthcare environment.
-

-
 New Grad and Newly Licensed Nursing Program
New Grad and Newly Licensed Nursing ProgramAs new grad or newly licensed RN, explore the rotational programs at our hospitals.
-
 Learn more about Nursing at BILH
Learn more about Nursing at BILHExplore the diverse and rewarding nursing opportunities at BILH, where you can make a meaningful impact on patient care while growing your skills in a supportive and innovative healthcare environment.
-
 Explore Upcoming Events
Explore Upcoming EventsStay informed and engaged by exploring the upcoming BILH events, where you'll have the opportunity to connect with colleagues, expand your professional network, and gain insights into the latest advancements and trends in healthcare.
-
 Learn more about Operating Room roles at BILH
Learn more about Operating Room roles at BILHExplore the many Operating Room nurse and surgical tech opportunities at BILH, where you can make a meaningful impact on patient care while growing your skills in a supportive and innovative healthcare environment.
-
 Explore open positions within our Radiology Team at BILH!
Explore open positions within our Radiology Team at BILH!Beth Israel Lahey Health has multiple opportunities to join the Radiology team. Join a work place that strives for excellence!
-

-
 Our Allied Health Team
Our Allied Health TeamLearn more about Allied Health job opportunities
-
 Job Opportunities: Woburn, MA
Job Opportunities: Woburn, MALearn more about job opportunities at BILH in the Woburn, Massachusetts area
-

Why join Beth Israel Lahey Health?
If you’re looking for a career where you can make a difference and explore your potential, Beth Israel Lahey Health is the place you belong. Our system includes a network of hospitals, physician practices, outpatient centers, and other healthcare facilities and we offer a broad range of careers in direct patient care, environmental services, registration, finance and many other fields. We are focused on providing compassionate and personalized healthcare with a strong reputation for clinical excellence and research and offer diverse opportunities for career growth and development. Conveniently, we have many locations in communities across Eastern Massachusetts and Southern New Hampshire.
At Beth Israel Lahey Health, we see you for all that you are – your experience and your dreams. Explore our open opportunities and find out why so many have already chosen to join our team.
View All Opportunities