Changing health care
to improve quality of
life for all.
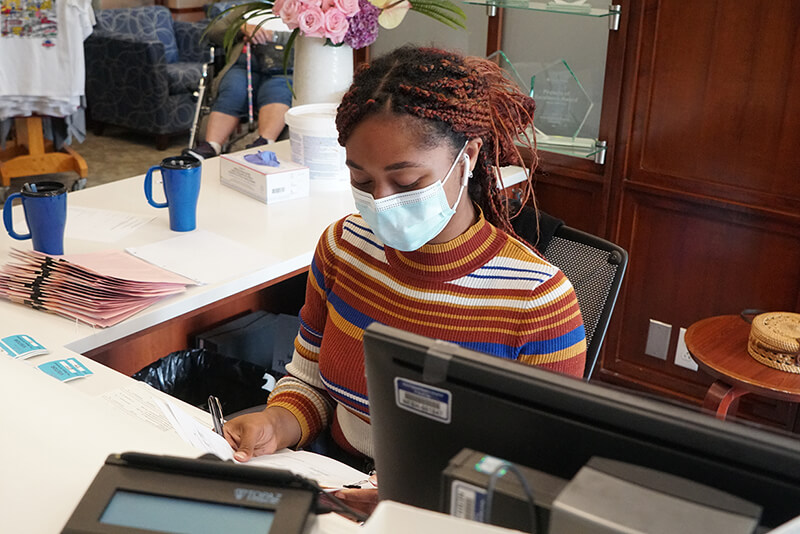
Beth Israel Lahey Health’s roots in providing top-quality health care date back nearly a century. We're fully committed to ensuring our patients receive the care they deserve. As a leading healthcare provider throughout New England, we aim to change the current state of health care for the better and make lasting improvements that guarantee access to our services.
Denial Specialist - Hybrid
Danvers, Massachusetts
Organization Facility: Beth Israel Lahey Health Behavioral Services Category: Billing, Collections, & Patient Financial Services Job ID: JR62213 Date posted: 11/08/2024Job Type: Regular
Time Type: Full time
Work Shift: Day (United States of America)
FLSA Status: Non-Exempt
When you join the growing BILH team, you're not just taking a job, you’re making a difference in people’s lives.
Identifies, reviews, and interprets third party payments, adjustments and denials. Initiates corrected claims, appeals and analyzes unresolved third party and self-pay accounts, initiating contacts and negotiating appropriate resolution (internal and external) to ensure timely and maximum payment. Manually and electronically applies insurance payments and works insurance overpayments, credits and undistributed balances. Works directly with the Billing Supervisor to resolve complex issues and denials through independent research and assigned projects.Job Description:
Benefits that start day-1!
Schedule: 40 Hours, days - Hybrid, with some onsite time in Danvers, MA
Essential Functions & Responsibilities:
Monitors days in A/R and ensures that they are maintained at the levels expected by management.
Analyzes work queues and other system reports and identifies denial/non-payment trends and reports them to the Billing Supervisor.
Ability to navigate the EHR billing system in order to identify paid claims or root cause of denial when assessing denials.
Responds to incoming insurance/office calls with professionalism and helps to resolve callers’ issues, retrieving critical information that impacts the resolution of current or potential future claims.
Establishes relationships and maintains open communication with third party payer representatives in order to resolve claims issues.
Reviews claim forms for the accuracy of procedures, diagnoses, demographic and insurance information, as well as all other fields on the CMS 1500.
Reviews and corrects all claims/charge denials and edits that are communicated via EHR, Explanation of Benefits (EOB), direct correspondence from the insurance carrier or others and uses information learned to educate PFS and office staff to reduce future denials and edits of the same nature. Initiates claim rebilling, written appeals or corrections and obtains and submits information necessary to ensure account resolution/payment
Evaluates delinquent third party accounts and processes based on established protocols for review, payment plan or write-off.
Reviews/updates all accounts for write-offs and refunds.
Reviews and follows through on all insurance credit balances through take back initiation, refund initiation, and/or payment re-application.
Keeps informed of all federal, state, and managed care contract regulations, maintains working knowledge of billing mechanics in order to properly ascertain patients’ portion due.
Completes all assignments per the turnaround standards. Reports unfinished assignments to the Billing Supervisor.
Handles incoming department mail as assigned.
Maintains appropriate audit results or achieves exemplary audit results. Meet productivity standards or consistently exceeds productivity standards.
Provides and promotes ideas geared toward process improvements within the Central Billing Office.
Assists the Billing Supervisor with the resolution of complex claims issues, denials, appeals and credits.
Works with cash team to resolve unapplied cash.
Completes projects and research as assigned.
Qualifications & Education:
High school diploma required, business school graduate preferred.
2-3 years’ experience in the billing services and denial management. Experience with automated receivable software necessary.
Ability to maintain a high level of confidentiality and relate to staff in a professional and patient manner.
Ability to demonstrate openness and flexibility to adapt to unplanned situations. Able to work cooperatively and in a fashion that promotes team building.
Computer literate in standard desktop applications such as Windows, Word, and Excel.
As a health care organization, we have a responsibility to do everything in our power to care for and protect our patients, our colleagues and our communities. Beth Israel Lahey Health requires that all staff be vaccinated against influenza (flu) and COVID-19 as a condition of employment. Learn more about this requirement.
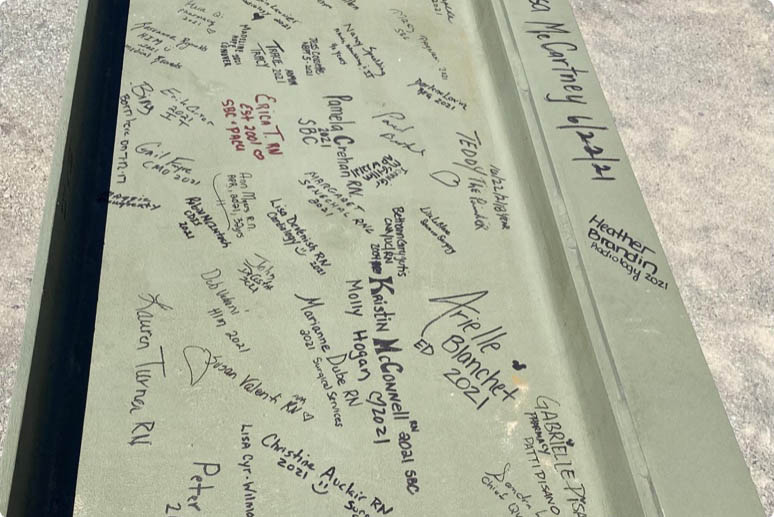
More than 35,000 people working together. Nurses, doctors, technicians, therapists, researchers, teachers and more, making a difference in patients' lives. Your skill and compassion can make us even stronger.
Equal Opportunity Employer/Veterans/Disabled
Featured Jobs
-

-

-

-

-
 Check out Benefits at BILH
Check out Benefits at BILHDiscover the outstanding BILH benefits that await you, encompassing competitive compensation packages, healthcare coverage, and a range of wellness programs designed to support your overall well-being.
-

-

-

-

-

-

-

-

-
 Learn more about Nursing at BILH
Learn more about Nursing at BILHExplore the diverse and rewarding nursing opportunities at BILH, where you can make a meaningful impact on patient care while growing your skills in a supportive and innovative healthcare environment.
-
 New Grad and Newly Licensed Nursing Program
New Grad and Newly Licensed Nursing ProgramAs new grad or newly licensed RN, explore the rotational programs at our hospitals.
-
 Learn more about Nursing at BILH
Learn more about Nursing at BILHExplore the diverse and rewarding nursing opportunities at BILH, where you can make a meaningful impact on patient care while growing your skills in a supportive and innovative healthcare environment.
-
 Explore Upcoming Events
Explore Upcoming EventsStay informed and engaged by exploring the upcoming BILH events, where you'll have the opportunity to connect with colleagues, expand your professional network, and gain insights into the latest advancements and trends in healthcare.
-
 Learn more about Operating Room roles at BILH
Learn more about Operating Room roles at BILHExplore the many Operating Room nurse and surgical tech opportunities at BILH, where you can make a meaningful impact on patient care while growing your skills in a supportive and innovative healthcare environment.
-

-
 Explore open positions within our Radiology Team at BILH!
Explore open positions within our Radiology Team at BILH!Beth Israel Lahey Health has multiple opportunities to join the Radiology team. Join a work place that strives for excellence!
-

-
 Our Allied Health Team
Our Allied Health TeamLearn more about Allied Health job opportunities
Why join Beth Israel Lahey Health?
If you’re looking for a career where you can make a difference and explore your potential, Beth Israel Lahey Health is the place you belong. Our system includes a network of hospitals, physician practices, outpatient centers, and other healthcare facilities and we offer a broad range of careers in direct patient care, environmental services, registration, finance and many other fields. We are focused on providing compassionate and personalized healthcare with a strong reputation for clinical excellence and research and offer diverse opportunities for career growth and development. Conveniently, we have many locations in communities across Eastern Massachusetts and Southern New Hampshire.
At Beth Israel Lahey Health, we see you for all that you are – your experience and your dreams. Explore our open opportunities and find out why so many have already chosen to join our team.
View All Opportunities