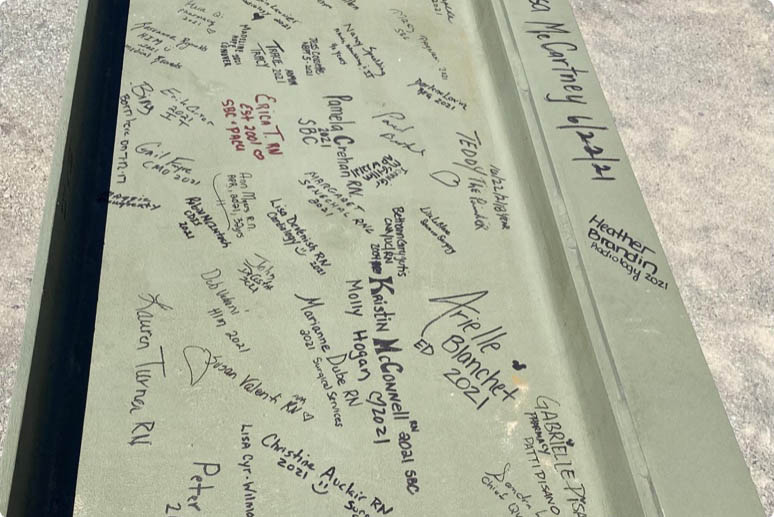
Learn more about working at Beth Israel Deaconess Hospital Plymouth
Care Transitions Jobs
Plymouth, Massachusetts
Organization Facility: Beth Israel Deaconess Hospital Plymouth Category: Billing, Collections, & Patient Financial Services Job ID: JR80537 Date posted: 07/01/2025Job Type: Regular
Time Type: Full time
Work Shift: Day (United States of America)
FLSA Status: Non-Exempt
When you join the growing BILH team, you're not just taking a job, you’re making a difference in people’s lives.
Job Description:
Are you a case management/utilization review professional passionate about improving care delivery and patient outcomes? Beth Israel Deaconess Hospital-Plymouth is expanding its Care Transitions Department and seeking an experienced Manager of Utilization Review & Denials Management and Utilization ReviewNurses to join our dedicated team. As a key part of our hospital’s commitment to quality, safety, and system efficiency, the Care Transitions team plays a vital role in ensuring seamless, patient-centered care.
_______________________________________
RN – Utilization Review
This role is ideal for nurses with strong documentation review skills and a deep understanding of reimbursement systems. You will manage concurrent reviews, appeal clinical denials, and support accurate level-of-care determinations.
Key Functions:
• Conduct concurrent and retrospective reviews for level of care and continued stay
• Lead appeals of clinical denials and collaborate with physician advisors
• Coordinate peer-to-peer reviews between providers and insurers
• Collect data and support denial prevention strategies
• Integrate clinical and reimbursement knowledge for optimal outcomes
________________________________________
RN Case Manager – Emergency Department UR & Discharge Planning
This position focuses on real-time discharge coordination and level-of-care review. You'll collaborate closely with physicians, nurses, patients, and community partners to ensure appropriate transitions of care from the Emergency Department and inpatient units.
Key Functions:
- Perform admission reviews and assign level of care using InterQual criteria
- Develop and manage individualized discharge plans and acts as a liaison between ED and post-acute providers
- Ensure compliance with Medicare, Code 44, and reimbursement regulations
- Address social determinants and high-risk cases in partnership with Social Work
- Advocate for safe, patient-centered discharges with strong documentation
________________________________________
Requirements for Both Roles:
- Current RN license in Massachusetts
- Minimum 3 years recent acute care experience
- Case management or utilization review experience within the last 3 years
- Proficiency in InterQual required
- CCM, ACM, or other case management certification preferred or in progress
________________________________________
Manager – Utilization Review & Denials Management
This role is ideal for a Manager with strong clinical knowledge, leadership skills, and a passion for innovation in Utilization Review & Denials Management who wants to make a tangible impact on both patient outcomes and organizational performance.
Key Functions:
- Oversee daily operations and directs staff performance regarding Utilization Review and the analysis, resolution, monitoring, and reporting of clinical denials
- Maintains a database to track level of care determinations and status of completion
- Consistently analyzes data and identifies trends/root causes of denials in order to strategically develop process improvement plans for identified deficiencies
- Participate on the UR Committee and adheres to HIPAA policies and procedures
- Participate regularly in meetings with stakeholders, including hospitalists, ED physicians, etc., to provide education and prevention strategies.
As a health care organization, we have a responsibility to do everything in our power to care for and protect our patients, our colleagues and our communities. Beth Israel Lahey Health requires that all staff be vaccinated against influenza (flu) as a condition of employment.
More than 35,000 people working together. Nurses, doctors, technicians, therapists, researchers, teachers and more, making a difference in patients' lives. Your skill and compassion can make us even stronger.
Equal Opportunity Employer/Veterans/Disabled
Related Jobs
-

-

-

-

-
 Check out Benefits at BILH
Check out Benefits at BILHDiscover the outstanding BILH benefits that await you, encompassing competitive compensation packages, healthcare coverage, and a range of wellness programs designed to support your overall well-being.
-

-

-

-

-

-
 Saved Jobs
Saved JobsView and manage your saved jobs
-

-
 Learn more about Nursing at BILH
Learn more about Nursing at BILHExplore the diverse and rewarding nursing opportunities at BILH, where you can make a meaningful impact on patient care while growing your skills in a supportive and innovative healthcare environment.
-

-
 New Grad and Newly Licensed Nursing Program
New Grad and Newly Licensed Nursing ProgramAs new grad or newly licensed RN, explore the rotational programs at our hospitals.
-
 Learn more about Nursing at BILH
Learn more about Nursing at BILHExplore the diverse and rewarding nursing opportunities at BILH, where you can make a meaningful impact on patient care while growing your skills in a supportive and innovative healthcare environment.
-
 Explore Upcoming Events
Explore Upcoming EventsStay informed and engaged by exploring the upcoming BILH events, where you'll have the opportunity to connect with colleagues, expand your professional network, and gain insights into the latest advancements and trends in healthcare.
-
 Learn more about Operating Room roles at BILH
Learn more about Operating Room roles at BILHExplore the many Operating Room nurse and surgical tech opportunities at BILH, where you can make a meaningful impact on patient care while growing your skills in a supportive and innovative healthcare environment.
-
 Explore open positions within our Radiology Team at BILH!
Explore open positions within our Radiology Team at BILH!Beth Israel Lahey Health has multiple opportunities to join the Radiology team. Join a work place that strives for excellence!
-

-
 Our Allied Health Team
Our Allied Health TeamLearn more about Allied Health job opportunities
-
 Job Opportunities: Woburn, MA
Job Opportunities: Woburn, MALearn more about job opportunities at BILH in the Woburn, Massachusetts area
-

Why join Beth Israel Lahey Health?
If you’re looking for a career where you can make a difference and explore your potential, Beth Israel Lahey Health is the place you belong. Our system includes a network of hospitals, physician practices, outpatient centers, and other healthcare facilities and we offer a broad range of careers in direct patient care, environmental services, registration, finance and many other fields. We are focused on providing compassionate and personalized healthcare with a strong reputation for clinical excellence and research and offer diverse opportunities for career growth and development. Conveniently, we have many locations in communities across Eastern Massachusetts and Southern New Hampshire.
At Beth Israel Lahey Health, we see you for all that you are – your experience and your dreams. Explore our open opportunities and find out why so many have already chosen to join our team.
View All Opportunities